Professional Medical Billing Services That Deliver Results
Health and Billing's medical billing services eliminate the complexity of managing your practice's revenue cycle internally. Our HIPAA-certified specialists combine advanced technology with deep healthcare industry knowledge to ensure maximum reimbursements while maintaining complete federal compliance.
We understand that every claim represents the financial foundation that keeps your practice running and allows you to focus on delivering exceptional patient care. Our dedicated billing teams treat your revenue with the same attention and expertise you provide to your patients.
Take the first step toward financial peace of mind.
CALL (386) Billing ( 386 245 5464)
Get Your Free Review
Medical Billing Services That Maximize Your Revenue!
Do you know approx $125 billion slips away every year in the U.S. because of billing errors? Yet most of it is recoverable!
Stop losing money to denials, delays, and compliance risks…
At Health and Billing, we combine advanced technology with expert oversight to help practices recover more revenue, reduce rejections, and speed up reimbursements
100% HIPAA-compliant processes that safeguard your practice
Optimized claim accuracy to cut rejections and denials
Accelerated payment cycles that improve your cash flow
Revenue-focused strategies for long-term financial stability
Start Optimizing Your Billing Today
Every denied claim is money left on the table. At Health and Billing, we help practices recover up to 35% more revenue, slash denials to under 2%, and cut A/R days by nearly half. All with 100% HIPAA-compliant systems
What Health and Billing Offers?
Unlike companies that simply “process claims,” Health and Billing delivers complete Revenue Cycle Management (RCM).
We cover every stage from patient intake and eligibility verification to medical coding, claims submission, denial management, patient collections, and financial reporting.
With us, your billing isn’t just managed. It is optimized for YOUR growth and MORE revenue!
Complete RCM Coverage
We offer, all-in-one RCM. We handle eligibility verification, prior authorizations, medical coding, medical audits, denial appeals, AR recovery, patient collections, and payer credentialing.
A 360° solution that ensures no revenue is left behind!
98–99% Clean Claim Rate
Every claim is scrubbed through 3 layers of validation with ANSI X12-837 EDI standards before submission.
Thus, drastically reducing rejections.
20–35% Revenue Uplift
Our clients consistently see double-digit improvements in collections. We use optimized coding (CPT, ICD-10-CM, HCPCS Level II) and payer-specific edits.
AI-Driven Accuracy
Our experts go for predictive denial analysis powered by AI and machine learning to detect potential rejections before submission. It improves first-pass acceptance.
Full Legal & Data Compliance
Our workflows strictly adhere to:
- HIPAA (Health Insurance Portability and Accountability Act)
- HITECH Act for secure health IT usage
- SOC 2 Type II certified processes
- OIG Exclusion Checks for regulatory safety
- CMS guidelines for Medicare/Medicaid compliance
Technology-Enabled Solutions
We work seamlessly with leading practice management and EHR systems such as: Our workflows strictly adhere to:
- eClinicalWorks
- Epic Resolute
Faster Reimbursements
We shorten your A/R days by 30–40%, ensuring reimbursements arrive weeks earlier. Our advanced clearinghouse integrations process ERA and eligibility instantly.
Performance Metrics & Reporting
Get a clear overview of your practice’s financial performance with the KPI Dashboard. We identify and report improvement opportunities and implement strategies that scale effectively.
Bills Collection & 24/7 Expert Support
Access a comprehensive summary of all medical bills, including status updates. We provide 24/7 hands-on support to resolve any billing issues quickly.
KPI Dashboard
Track key performance indicators in real time, including copays collected, accounts receivable per payer, and overall financial health. Know exactly where your revenue stands at a glance.
Schedule a Free Discussion!
Health & Billing
We Ensure: ACCURACY. COMPLIANCE. MAXIMUM REIMBURSEMENT.
WHO WE SERVE?
Solo and multi-provider practices
Small clinics through large hospitals
Specialty centers (e.g., imaging, ambulatory surgery)
Labs, FQHCs, and DME providers
Practices across more than 50 medical disciplines.


Did you know the average denial rate in healthcare is 10%?
At Health & Billing, we help practices dramatically reduce denials..
And every 1% drop in denials translates into THOUSANDS of dollars in recovered revenue each year.
Stop leaving money on the table and start getting paid what you deserve!
What You Will Get With Our Medical Billing Services
Credentialing & Enrollment
Get listed with all major payers quickly and avoid costly delays.
Eligibility & Pre-Authorization
Real-time insurance verification ensures coverage before services are delivered.
Medical Coding & Charge Entry Services
Certified coders (CPC, CCS-P) with deep specialty expertise use AI-driven checks for CPT, ICD-10, and HCPCS accuracy.
Claim Submission & Scrubbing
Electronic claim submission (ANSI X12-837) with 3-layer scrubbing for maximum first-pass acceptance.
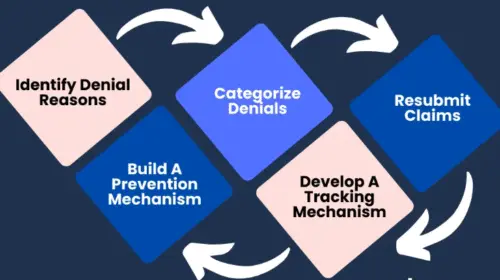
Denial Management & Appeals
Denials are analyzed, corrected, and resubmitted within 24–48 hours. Complex cases are appealed aggressively.
Accounts Receivable (A/R) Recovery
We follow up relentlessly, recovering aged claims—even those 120+ days old.
Patient Billing & Collections
Clear statements, online payment portals, and compassionate patient support reduce friction and improve collections.
Advanced Analytics & Reporting
Dashboards with KPIs such as denial rates, net collections, payer mix, and cost-to-collect.
Quarterly Audits & Fee Schedule Optimization
Identify underpayments, benchmark against peers, and adjust your fees for maximum reimbursement.
Seamless EHR & Practice Management Integration
Works smoothly with top EHRs like Epic, Athenahealth, Kareo, AdvancedMD, eClinicalWorks, and Allscripts.
Why Outsource Medical Billing Services?
Medical billing is the bridge between patient care and provider reimbursement. Accurate billing transforms medical billing from a time-consuming task into a strategic advantage!
By partnering with our trusted medical billing services, you can ensures you receive timely and fair payment for your services, while reducing errors that can cause costly delays or denials.
Minimize your Administrative Burden. With Improven Accuracy
Let’s discuss and EARN more with our Medical Billing Services!
FAQs
What sets Health and Billing’s medical billing service apart?
We provide end-to-end Revenue Cycle Management (RCM). From eligibility verification, medical coding (CPT, ICD-10-CM, HCPCS Level II), claim scrubbing, denial management, AR recovery, to patient collections, we are an all-in-one solution.
Are you compliant with regulations?
How do you improve revenue and reduce denials?
Through AI-powered claim validation, predictive denial analysis, and payer-specific edits, we achieve 98–99% clean claims, reduce denials below 2%, and recover up to 35% more revenue.
Which specialties are supported?
How do you monitor financial performance?
Our KPI dashboards track AR per payer, copays, bill statuses, and revenue trends. Performance metrics allow actionable insights for cash flow optimization and scalable practice growth.
Is your service scalable?
How do you handle patient billing?
We automate insurance eligibility checks, co-pay collection, and patient balance reminders to reduce AR days. Patients receive transparent statements, improving collections without friction.
How quickly can results be seen?
Health & Billing Brings
Hope, Health & Harmony
To Your Healthcare Practice
So, You can focus on what’s more important: Patient Care!
Reduced Administrative Burden | Improved Cash Flow | 100% HIPAA-compliance
Cost Efficiency | Certified medical coders and credentialing specialists | Scalable Solution
